
I joined the Strategy Office at Cleveland Clinic in 2016 to provide a human-centered design (HCD) and patient experience (PX) lens to business development.

Following are three examples of service line delivery challenges I worked on.
Colorectal Cancer Navigation

Colorectal cancer is the third most commonly diagnosed cancer and the third most common cause of cancer-related death in both men and women in the United States (1). For patients and their loved ones, it can feel overwhelming and frightening. Cleveland Clinic sought to empower people during this life changing experience and bring a “patients-first” approach to care.
My patient-centered work led to the creation of a new patients’ handbook, which was met with widespread enthusiasm by patients, and which was subsequently adopted by a total of three cancer specialty teams.
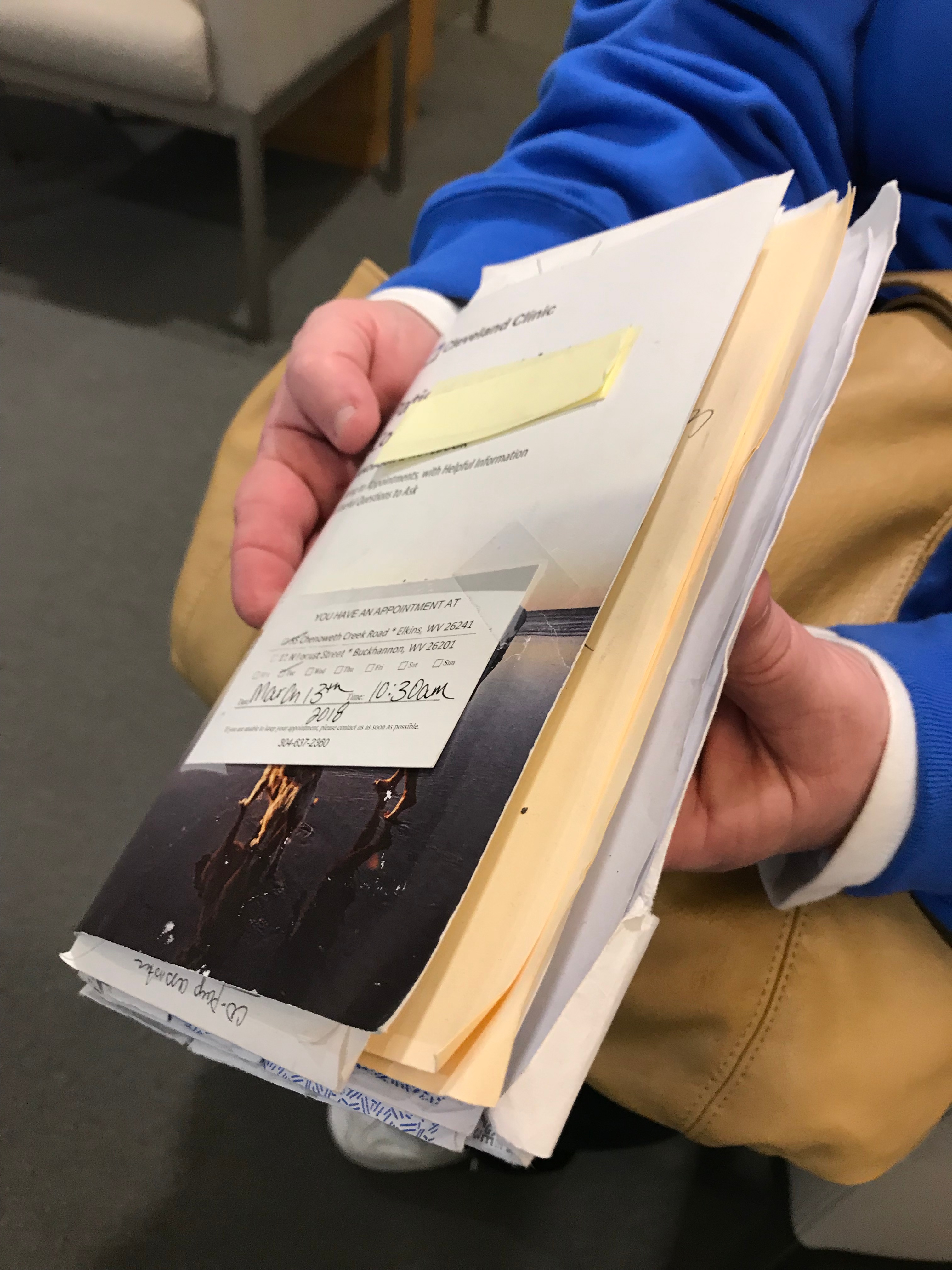
Up to that point, thick binders of printed material developed by doctors were handed to patients, making what was already a scary diagnosis even more intimidating. Illustrations of suture methods and colostomy types demonstrated the physicians’ expertise, but failed to connect with patients’ lived experience. There had to be a better way.

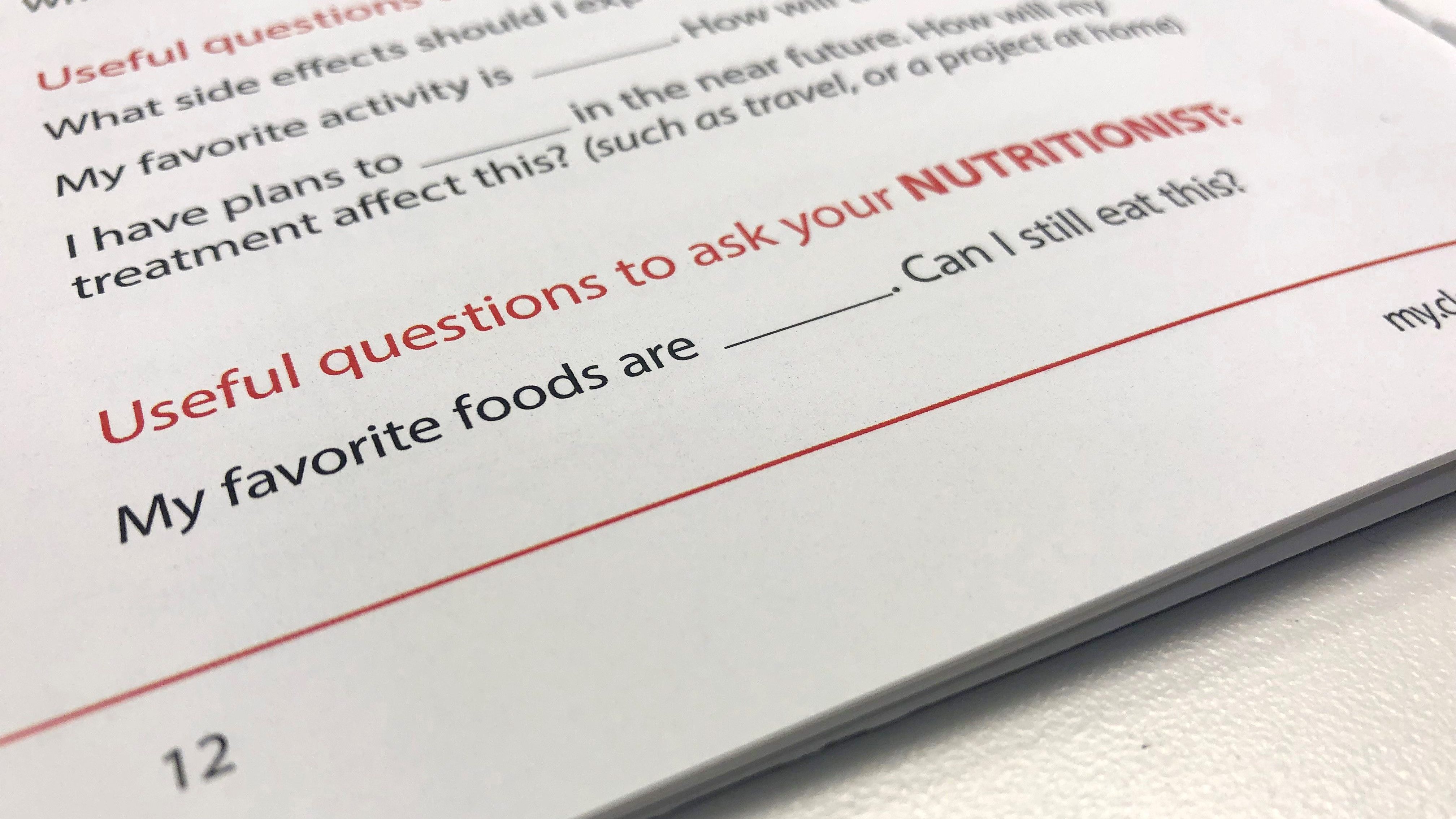
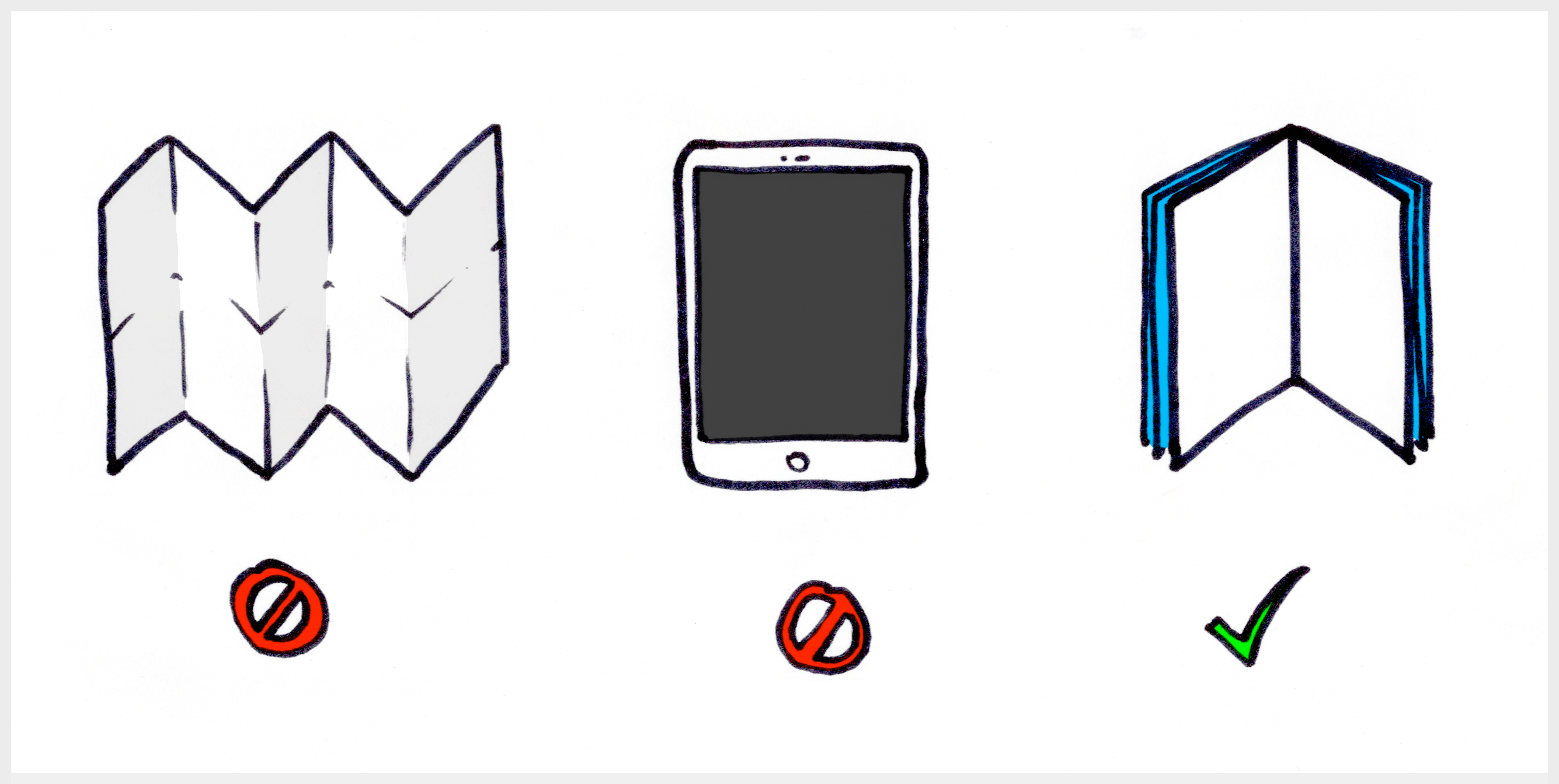
Earlier research identified patient navigation as a primary means to support patients and families. I prototyped three designs to guide people through conversations with their clinical care providers, and tested them with patients who were in the process of colorectal cancer treatment. A simple “patient’s handbook” emerged as the clear favorite with patients. But the handbook was only part of the equation.
The cancer team was simultaneously developing a “patient navigator” role, but they didn’t have a clear sense of how this position could be fully utilized. The patient handbook became the perfect anchor on which to base those interactions, providing a boundary object to bridge the patient’s and care team’s contexts.
Patients loved using the handbook, and Cleveland Clinic’s expert team of graphic designers and content specialists turned the prototype into a fully developed, integral component of care. We also developed a simple webpage with much of the same information in the printed handbook. The model was subsequently adopted by two other cancer divisions with great enthusiasm.
(1) Source: American Cancer Society, link
Enterprise Weight Management
In 2018, Cleveland Clinic boasted over 150 programs to help patients manage their weight. Despite this, 73% of patients were clinically obese or overweight, reflecting national statistics. In practice, most of Cleveland Clinic’s weight management programs were disjointed, and some had competing treatment advice. Executive leadership engaged my team to bring clear, consistent protocols and a governance model to the different programs.
Our work resulted in a unified stepwise protocol, a simplified EHR process, and the establishment of the Enterprise Weight Management Center for program governance and accountability.
Our team began by auditing the existing weight management offerings and connecting with over 40 department leaders to learn about their programs. We interviewed 12 patients who had used Cleveland Clinic to achieve their weight loss goals. Using these insights, my team worked with executive leaders to configure oversight mechanisms across 18 hospitals providing weight management care in Northeast Ohio.

One important insight we learned from our patient interviews was that beyond any medical interventions, patients had to change their entire mindset about managing weight. Some people mentioned it directly, and others showed us things they did around their homes to support new ways of thinking about weight management (most of our interviews were conducted on-site, where people lived.)
In leadership meetings at Cleveland Clinic we showed video clips from the patient interviews, and physician partners saw how their advice played out in their patients’ day to day lives. It was powerful and moving for my colleagues to hear how their guidance was interpreted by patients and the influence they had (or sometimes didn’t have).
Weight management care delivery is complex, so I created a service blueprint to help clinicians and administrators see how patients evaluate, adopt, and navigate the system. It illustrated where providers integrate into the process, the role support staff plays, and how our backend systems support results. I printed the blueprint on a 4 ft. x 15 ft. poster to hang up during our working sessions, to keep the team oriented to the many levers we control to affect change.

Patients we interviewed told us about what worked for them, and what held them back. Some factors, like social determinants of health (SDH) were better suited to being addressed by other initiatives. But we could control for things like a common care pathway, an electronic health record (EHR) documentation protocol, and improved patient information on the Clinic website.
After nine months of assessment, asking hard questions, and listening closely to answers, what emerged was a holistic, patient- and physician-informed approach to weight management across our growing healthcare system. We created a step-wise model of care, designed patient-facing digital resources, and appointed the first Director of Enterprise Weight Management.

As a testament to the power of human-centered design, the doctor chosen to lead the new program was not an endocrinologist or a bariatric surgeon (practitioners who drove important outcomes for particular user groups), but a clinical psychologist, whose practice underpinned the success of nearly all the patients we interviewed.
This work was co-led by myself and my brilliant colleagues at Cleveland Clinic Strategy Office, Judith Morris-Barrie, MBA, and Allison Lee Grazia, a graduate intern from Case Western Reserve University, whose contributions and subject matter expertise were invaluable to the success of this work. I subsequently co-authored a white paper on this research which was published in the Southern Medical Journal.
Pediatric Asthma Care
Many kids suffering from asthma grow out of it, but Cleveland Clinic wanted to improve the service experience of those whose asthma follows them into adulthood. By considering people’s life journeys, Cleveland Clinic aimed to provide more holistic care to millions of patients. We started by looking at pediatric asthma care.
Our work resulted in enhanced public school partnerships for pediatric asthma care in seven area school districts in northeast Ohio.
My team began by interviewing sixteen kids and their families about living with and managing their asthma. We noticed how some kids felt less held back by the symptoms of asthma and how some were more proactive about asthma management. Four profiles emerged that characterized how people approached their care, which provided clues as to how to tailor interventions.

Link to persona framework (requires password).
Next we talked with healthcare providers at a local elementary school and at Cleveland Clinic medical centers to learn about the clinical approaches they used. They validated the patient types we’d identified and we workshopped ideas for ways to meet different patients where they were.
My team created storyboards to imagine how different concepts might play out. This helped identify the myriad of stakeholders and touch points for each intervention. We conducted an Effort x Impact exercise to determine which interventions could be piloted with existing resources, and decided to focus on school nurses who provided asthma care.
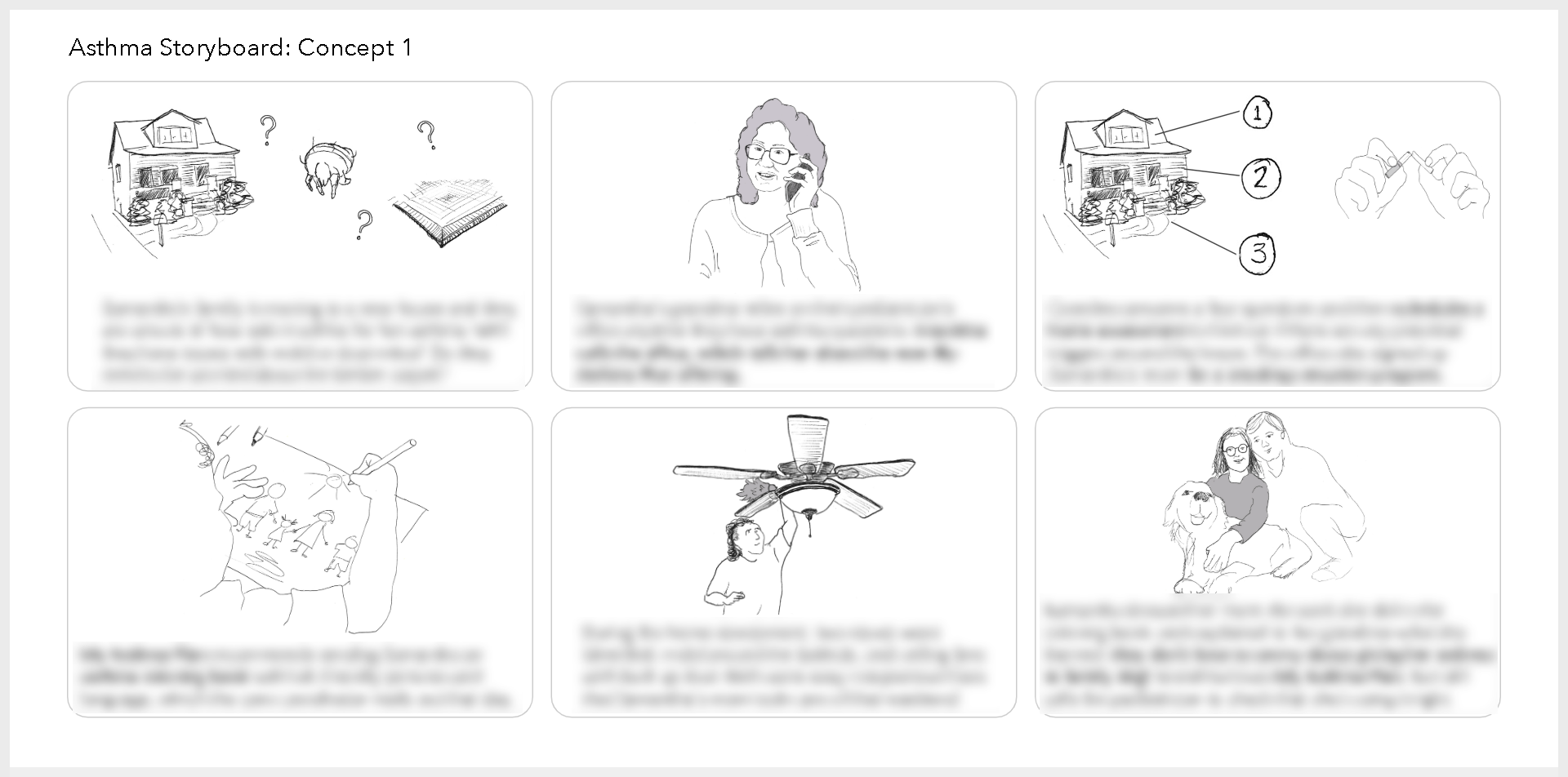
Link to storyboards (requires password).
We worked with school administrators and Cleveland Clinic clinicians to coordinate how asthma care could be integrated into schools with limited resources, and how families could be more involved with students’ asthma resources.
Today, Cleveland Clinic Children’s School–Based Health program offers a mobile, full-service pediatric office staffed with healthcare professionals. It visits schools in seven area school districts and daycares, providing care for kids in grades K through 12. When the unit is not at a particular school, kids can have virtual visits with providers.
Additional Achievements
- Represented Cleveland Clinic at the inaugural and second gatherings of what became the Institute for Healthcare Delivery Design. The group was co-founded by Kim Erwin, Hugh Musick, and Jerry Krishnan, MD as a forum for defining how human-centered design can impact healthcare.
The consortium brought together designers and clinicians from leading healthcare institutions across the US, including Mayo Clinic, Cleveland Clinic, Memorial Sloan Kettering Cancer Center, UT Austin, UPMC, and Optum. It has since developed further into the Equitable Healthcare Lab at the IIT Institute of Design in Chicago.

- Created an HCD playbook to define best practices, capabilities, expected outcomes and deliverables for future design endeavors. I’d like to credit my colleague, Elliott Wortham, for his invaluable contribution to this resource.
- Facilitated several breakout sessions at the annual Patient Experience Summit hosted by Cleveland Clinic between 2017-19. (see photo, below, and on this site’s homepage)
- Planned and built a 900-sq. ft. “kiva room” collaboration space to facilitate design thinking workshops. (see photos, below)
- Produced intro videos for hospital acquisitions in northeast Ohio and southern Florida and for Cleveland Clinic “MedTalks” innovation series.
- Presented a poster at the HXD Conference hosted by Mad*Pow in Cambridge, Mass in 2018.
- Mentored the Strategy Office’s first design intern, Allison Lee Grazia, who did amazing work developing a detailed journey map of patients navigating weight management.
- Designed and facilitated several Patient Advisory Board workshops to inform a range of enterprise initiatives, co-hosted by my wonderful colleague, Amy Szabo.
- Developed and led “Sketch Class” for MBAs and healthcare administrators to teach sketching techniques for brainstorming and lateral thinking.
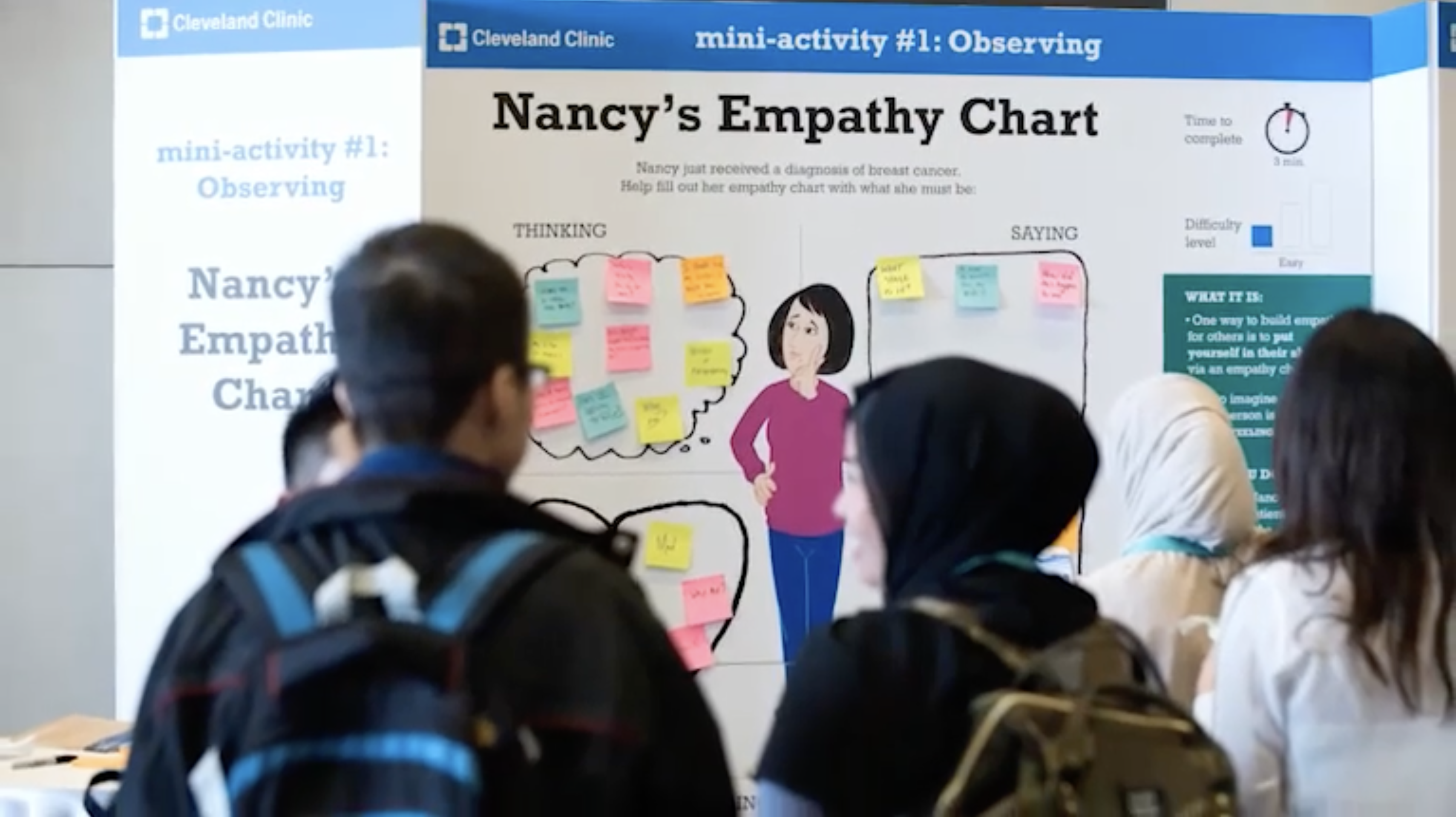
I created this Patient Empathy board as part of a series of interactive mini-activities for attendees at the 2017 Patient Experience Summit. Photo credit: Cleveland Clinic.

This is a scale model of the “kiva” collaboration room I designed and built with architects at Cleveland Clinic. We used movable furniture, wheeled whiteboards, and adjustable lighting to create a reconfigurable space to accommodate different types of engagements from small working sessions to larger group workshops.

Skills and methods: Presentations · Journey maps · User behavior · Workshops · Personas · Group facilitation · Visual communication · Process design · Team leadership · Constructive feedback · Co-creation · Service blueprints · Design research · Creativity skills · Video production · Design thinking
Project Statistics
Role: Service Designer (Associate Strategy Partner III)
Dates: Nov. 2016 – March 2020
Client: this was my in-house role at Cleveland Clinic‘s Strategy Office
Top image by Andrew Tanglao on Unsplash


